Plantar Fasciitis
 People experiencing extremely painful and sometimes debilitating heel pain might be suffering from plantar fasciitis. This condition affects millions worldwide daily, making it one of the most typical causes of heel pain.
People experiencing extremely painful and sometimes debilitating heel pain might be suffering from plantar fasciitis. This condition affects millions worldwide daily, making it one of the most typical causes of heel pain.
In this informative summary, we’ll dive into the root causes of this condition, how to spot its telltale signs, the various treatment options available, and the smart steps you can take to minimize future flare-ups. Read on to discover valuable insights and take control of your foot health.
If you have plantar fasciitis, contact Sforzo | Dillingham | Stewart Orthopedics + Sports Medicine to schedule a consultation with one of our physicians. Our team of highly trained medical experts can identify and treat your medical problems.
What is Plantar Fasciitis?
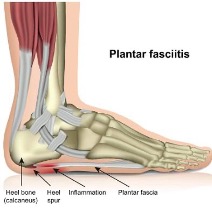
The severe inflammation of the plantar fascia, found at the sole of your foot, is frequently caused by plantar fasciitis. It is a sign that you have this condition if you experience persistent heel discomfort.
The plantar fascia is a stout, fibrous connection that stretches from your heel to the toes. Comparable to a ligament, it’s like an elastic band that connects all of the bones in your foot and produces the arch on its underside.
Excessive pressure and straining of the plantar fascia leads to plantar fasciitis, which manifests as swelling and pain that can make even walking challenging. It’s common to experience this condition on one foot at a time. However, both feet can be affected simultaneously.
A study found that plantar fasciitis is a widespread source of heel discomfort, affecting nearly two million US citizens. Resulting in more than one million visits to medical professionals for diagnosis and treatment annually.
Symptoms of Plantar Fasciitis
The most notable symptoms of plantar fasciitis are given below:
- Searing pain in your heel
- Pain radiating from the arch of your foot
- Rigidness and tightness surrounding your Achilles tendon
- Inflammation around the heel region
Causes of Plantar Fasciitis
Plantar fasciitis is caused by anything that places strain on the plantar fascia, including:
- Spending extended periods standing
- Participating in sports
- Exercising without proper stretching and warming up
- Wearing ill-suited shoes such as flip flops or flat sneakers with no arch support
- Walking barefoot at home
Plantar Fasciitis – Risk Factors
 Plantar fasciitis is likely to happen if you belong to one of the following categories.
Plantar fasciitis is likely to happen if you belong to one of the following categories.
- Habitual activities that stress your heel and the attached tissue – like long-distance running, ballet dancing, or aerobic dance – could lead to plantar fasciitis.
- Additionally, people between 40 and 60 are most prone to this affliction.
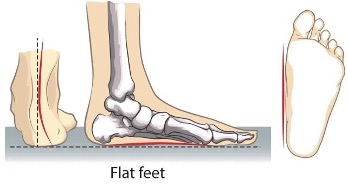
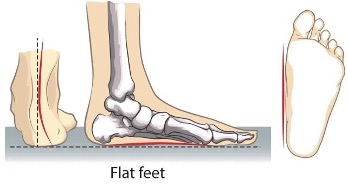
- If you have flat feet, a high arch, or an abnormal gait pattern, the weight distribution when standing can be impacted, and more pressure is exerted on the plantar fascia.
- Obesity can cause stress on your plantar fascia.
- Plantar fasciitis is more likely to affect those who spend most of their day on hard surfaces, such as industrial employees.
Diagnosis of Plantar Fasciitis

When diagnosing plantar fasciitis, your medical history and physical examination are considered. During the exam, tenderness in various areas of the foot will be assessed; this helps pinpoint the source of discomfort. Knowing where you feel pain is crucial to obtaining an accurate diagnosis.
Generally speaking, no tests are necessary to diagnose heel pain. However, if your healthcare provider suspects the issue may be more than plain old heel pain, an X-ray or MRI might be ordered. X-rays can reveal a bone spur on the heel bone. However, these spurs are frequently mislabelled as causing discomfort when this isn’t necessarily true in all cases – many people can have them without any soreness symptoms.
Plantar Fasciitis – Treatment
Non-Surgical Treatment
Plantar fasciitis can often be managed with simple, at-home treatments and OTC medications. In addition, your healthcare provider is available to provide suggestions that help relieve your symptoms and support your feet to prevent the risk of future recurrences.
Popular non-surgical remedies for plantar fasciitis pain relief include:
- Immobilization: The plantar fascia is less stressed when you wear a walking brace, also called a walking cast. How long you should utilize this sort of support device will be determined by your doctor.
- Wearing Supportive Shoes: Invest in reliable, comfortable shoes with built-in arch support. Avoid sandals, flip-flops, or other soft-sole footwear at all costs. Walking barefoot is an especially bad idea.
- Rest: Step away from sports or any activities which may have caused the plantar fasciitis for at least one week (or longer, if feasible). A pause to reflect will benefit your feet’s health in the long run.
- Icing Your Foot: Rexal your feet by icing them for 10-15 minutes every day, twice daily. To avoid harming the skin, wrap a cold water bottle in a thin towel and roll it across the bottom of your foot to soothe any inflammation.
- Orthotics: Increase the comfort of your shoes by adding inserts for additional arch support. Your provider can recommend pre-made, over-the-counter models or custom orthotics to precisely fit your foot’s shape. Either way, you will appreciate added support and cushioning.
Surgical Treatment
The actions mentioned above are usually all you need to overcome the pain caused by plantar fasciitis. Nonetheless, a few surgical procedures can be executed if necessary. These consist of Gastrocnemius Recession and Plantar Fascial Release, whereby your surgeon will lengthen the calf muscles or make small cuts on your fascia. Both aim at relieving the pressure present.
Surgery is rarely required when treating this condition, so ensure that other treatments have been exhausted before opting for surgery. Which sort of surgery is best for treating this problem will be explained to you by your orthopedic surgeon.
Plantar Fasciitis – Preventive Measures
 To avoid this condition, it’s crucial to keep your feet healthy. Here are some tips:
To avoid this condition, it’s crucial to keep your feet healthy. Here are some tips:
- Stretch before and after physical activity.
- Take breaks during intense exercise.
- Invest in supportive shoes.
- Avoid going barefoot on hard surfaces.
- Replace sneakers every 250-500 miles or 6-9 months.
Implementing these habits will help protect you against this common condition. Unfortunately, if you are prone to this condition genetically, it may be regrettably inevitable. However, taking certain measures can lessen the likelihood of getting this disease.
Contact our team of orthopedics and sports medicine experts at Sforzo | Dillingham | Stewart Orthopedics + Sports Medicine today to book a consultation with one of our physicians. We specialize in treating plantar fasciitis, fractured hips, spine injuries, and sports-related ailments with unparalleled care. Call us now at 941.378.5100 to book an appointment.









 People experiencing extremely painful and sometimes debilitating heel pain might be suffering from plantar fasciitis. This condition affects millions worldwide daily, making it one of the most typical causes of heel pain.
People experiencing extremely painful and sometimes debilitating heel pain might be suffering from plantar fasciitis. This condition affects millions worldwide daily, making it one of the most typical causes of heel pain.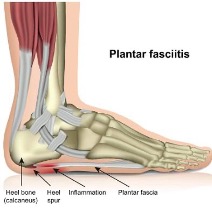
 Plantar fasciitis is likely to happen if you belong to one of the following categories.
Plantar fasciitis is likely to happen if you belong to one of the following categories.
 T
T










